Five Reasons Why AI Won’t Replace Radiologists
Even before the current AI and LLM revolution, radiologists were feared to be the first doctors replaced by automation. As both a radiologist and computer science enthusiast, here are five reasons why I believe that won’t happen.

Five Reasons Why AI Won’t Replace Radiologists
By Dr. Khaled Dostzada
Even before the current AI and LLM revolution, radiologists were often feared to be the first physicians replaced by automation. As someone who’s spent most of his life studying computer science — and now practices as a radiologist — I want to offer five key reasons why I believe AI won’t replace radiologists (or any other profession) anytime soon.
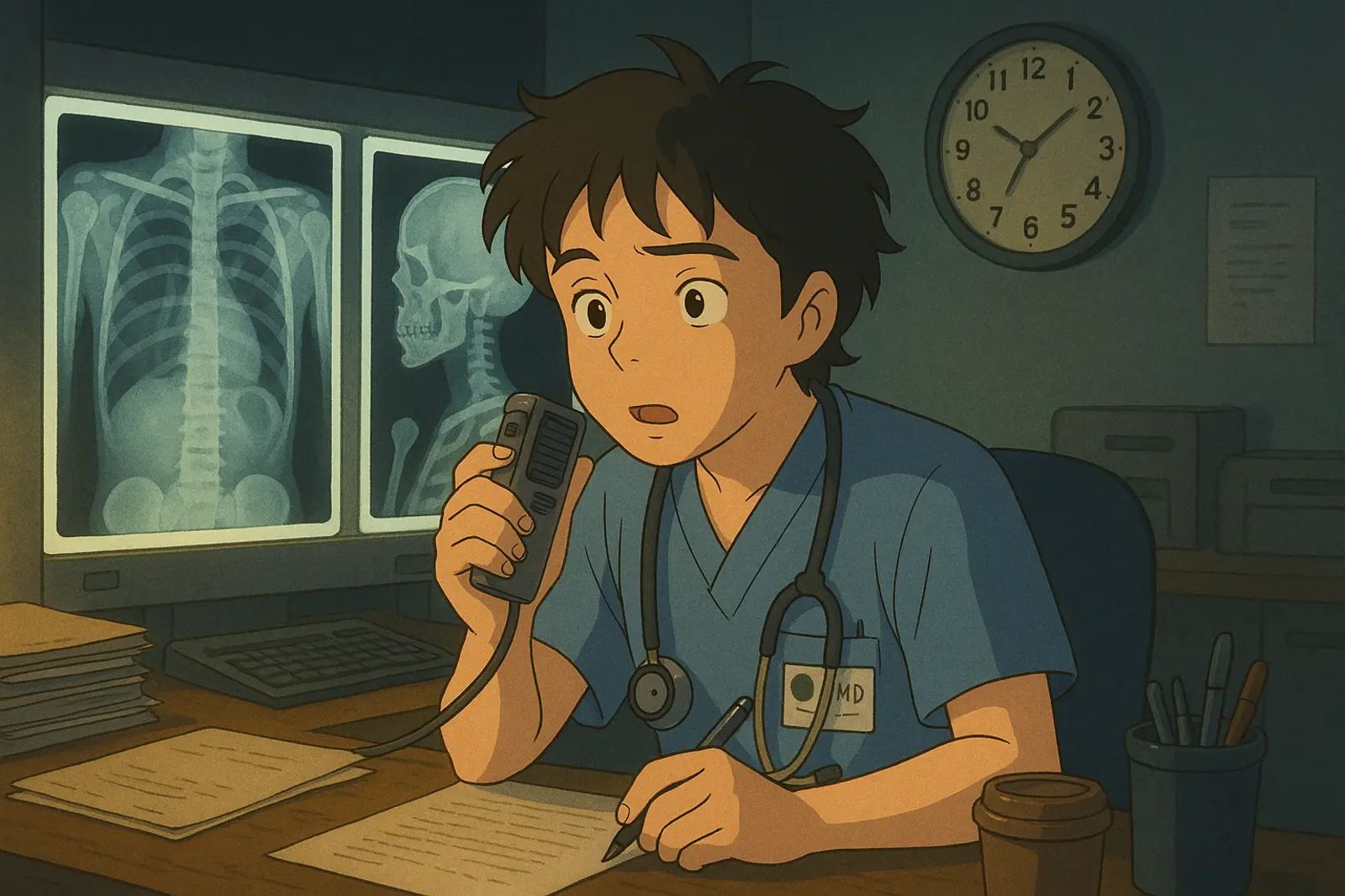
The stereotype of quiet introverts sitting in a dark room reading scans all day lends itself well to the narrative of the AI revolution.
From the outside, it’s easy to understand why radiology seems ripe for automation. The work appears data-heavy and image-based — perfect conditions for algorithms. So much so that a Nobel Prize-winning computer scientist once predicted radiologists would be obsolete in five years. That was nine years ago. Since then, both the number of radiologists and our workload have only grown.
1. Radiologists Are Clinicians — And Yes, We See Patients

Hard to believe, right? But despite the stereotypes, radiologists interact with patients — a lot.
Before there’s even an image on a screen, significant work has been done by radiologists and technologists — interpersonal work no neural network can replicate.
We perform image-guided procedures, manage contrast reactions, run stress tests, and take countless calls in the reading room. We also recommend follow-up imaging, relay critical findings, and coordinate care.
Behind every scan is a flurry of clinical decision-making, patient communication, and department-level coordination that machines can’t handle — and likely never will.
2. There’s More Than Enough Work for Both Humans and Machines
There’s a nationwide radiologist shortage, and it’s only worsening. Imaging volumes are exploding thanks to faster scanners and wider access to care, yet residency training slots remain limited as more senior radiologists retire.
Radiology often feels like running on a treadmill: you read 10 studies in four hours, and 20 more appear before you can catch your breath.
A 2024 Danish study showed that AI reading all normal chest x-rays only reduced workload by 20%. AI helps, but it’s no silver bullet. Imaging volume keeps growing, and we’re drowning in work — even with AI support.
3. Clinical Context Is Everything
AI is powerful, but it thrives on averages. Most hospitalized patients, however, are anything but average. Their clinical histories are complex, and prior surgeries often alter normal anatomy in unpredictable ways.
Many diseases share overlapping imaging features — the only way to differentiate them is by understanding clinical history.
As radiologists, we’re constantly digging through charts, reviewing surgical notes, comparing studies across years and modalities. Sometimes the key to a CT abdomen lies in an ultrasound of the neck from five years ago.
Doctors don’t treat datasets. We treat human beings, each with a unique story — a reality AI is far from understanding.
4. Everyone Wants to Be a Radiologist — Until It’s Time to Decide

Radiologists make decisions that profoundly impact lives — whether someone goes to surgery, loses a limb, or continues a pregnancy.
These decisions require accountability — someone willing to explain the reasoning and take responsibility.
Current AI systems often operate as opaque black boxes. They may output an answer that sounds confident but can’t explain how or why they reached it — a phenomenon known as AI hallucination.
In high-stakes medicine, someone has to make the final call, justify the diagnosis, and face the patient. That someone is — and should be — a human.
5. Humans and AI Complement Each Other

I know — it may sound like I’m overly critical of AI. The truth is, I love it. I’ve followed machine learning since 2014 and use AI tools daily at work.
Here’s what I’ve found: radiologists excel at contextual diagnosis and correlation. AI shines in pattern recognition, especially when findings are subtle, diffuse, or symmetric.
Take the image above. The bottom row shows a patient with diffuse cerebral edema — a critical condition. It looks almost identical to the normal scan above it, especially on a grainy machine. AI is excellent at catching these nuanced patterns.
But recently, I had a case where AI detected a brain bleed — and completely missed a carotid artery dissection. Why did I find it? Because I knew to look. Spontaneous brain bleeds and dissections often stem from the same cause: hypertension. That clinical knowledge isn’t in the pixels.
Final Thoughts
I’m incredibly excited about AI in radiology.
I don’t fear replacement — I welcome augmentation. AI will make us faster and more accurate, ultimately improving care for the patients we serve.
Some tools I’m especially excited about:
- LLM-powered report drafting: Pre-fill measurements and boilerplate language, so we can focus on interpretation.
- AI chart summarization: Instantly condense years of clinical notes into a relevant, concise summary.
- Automated lesion tracking: Precisely align scans and track changes over time without tedious measurements.
- AI-powered communication: Automatically notify physicians or patients about critical findings — and document it — so we can keep reading.
If anything, the future of radiology isn’t AI vs. radiologists — it’s AI with radiologists. And that’s a future I’m proud to be part of.
Share this post
Found this helpful? Share it with others!